
Clinical Vignette 74
A teenager developed persistent high fever (up to 39.5 degrees Celsius) two weeks after returning from a trip to a national park in Brunei. The other nine students and teacher-counsellor remained well other than occasional bouts of gastroenteritis. The school excursion had lasted a week, with two days spent camping in tents within the national park. All students had reported being bitten by many insects, especially mosquitoes, although malaria chemoprophylaxis was not used in accordance with international guidelines (Brunei has been declared malaria-free by the WHO since 1987).
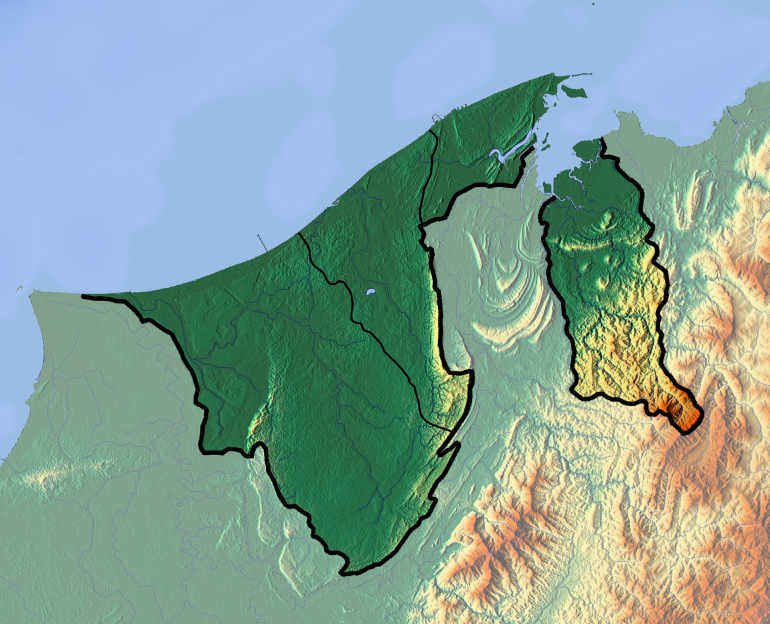
National park in Brunei: image obtained from Wikipedia
The young man had developed fever acutely, with mild headache but no other localising symptoms. He had visited two doctors over the course of 6 days without much relief, with antibiotics (amoxicillin/clavulanate) prescribed during the second visit. There was no other contact or travel history of note. Clinical examination was unremarkable. A full blood count showed mild thrombocytopenia (platelet count of 114) and mild anaemia (Hb of 12.8 g/dL), while LFT showed mild transaminitis.
Questions:
- What are the possible differential diagnoses?
- What other investigations should be performed?
[Updated 22 June 2017]
Given the timeline and exposure history, there are several possible differential diagnoses to consider. These include: typhus, leptospirosis, dengue (which will have nothing to do with the trip to Brunei – the incubation period is less than a week on average) and malaria. Although Brunei has been declared malaria-free since 1987, infections with Plasmodium knowlesi are commonly reported in north Borneo (which includes Sabah, Sarawak and Brunei). This was a key finding of the Monkeybar project led by Dr Timothy William and Dr Tsin Wen Yeo in Sabah.
This young man was prescribed doxycycline, and his fever had abated by the time the blood film report returned 36 hours later (it was sent to a private laboratory on a weekend) documenting the presence of 0.2% malaria parasitemia. He subsequently completed a short course of chloroquine as for P. knowlesi malaria. Note that optimal treatment for monkey malaria (P. knowlesi is a primate/macaque malaria parasite that only secondarily infects humans) is with an artemisin-based combination, as demonstrated in a convincing clinical trial by the Sabah-Singapore-Australia investigators.
Anything remarkable in the unremarkable examination and limited labs that you might be withholding?… presence of exanthem, conjunctival injection, missed visceromegaly, urinalysis abnormalities, peripheral blood smear, presence of blasts, etc. DDx: P. knowlesi (I feel manipulated by the invisible hand to include Plasmodium), Salmonellosis, leptospirosis, rickettsiosis, “arboviruses”, HUS, JRA, on and on – all in their forme fruste
LikeLike
The “invisible hand” of an experienced infectious diseases physician is highly accurate indeed. Clinical examination was indeed unremarkable – although “WNL” sometimes stands for “we never looked” rather than “within normal limits”.
LikeLike