Clinical Vignette 13
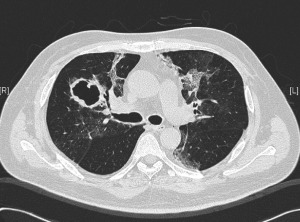
This is the same middle-aged man presented in the previous clinical vignette. He had undergone allogeneic stem cell transplantation (allo-HSCT) for underlying B-cell leukemia, with subsequent acute graft-versus-host disease (GVHD) of the liver. This was complicated 6 months later by RSV pneumonitis as previously described. His recovery was slow and required oxygen support even 3 weeks after the start of the RSV infection. A repeat CT showed cavities in both lung fields, with resolution of the prior ground-glass changes. These cavities appeared in the regions of the lungs previously affected by RSV. He was otherwise afebrile, with a slight cough and exertional dyspnea (requiring oxygen support) but has no other symptoms.
Question: What new complication has set in for this immunocompromised patient?
[Updated 28th December 2014]
The repeat CT thorax showed multiple irregular, thick-walled cavities in both lungs. Medscape has a nice article on the various differentials of cavitary lung lesions. Various bacterial, fungal and mycobacterial organisms are able to cause such changes in an immunocompromised patient, but the most likely cause in this particular setting is infection caused by a mould belonging to Aspergillus spp. This can be diagnosed indirectly via serum or broncho-alveolar lavage fluid testing for galactomannan – a component of the Aspergillus spp. fungal cell wall (although the former is not particularly sensitive), or biopsy of the wall of a cavity. Treatment upon confirmation of diagnosis is with antifungal therapy. Voriconazole is currently the drug of choice – amphotericin formulations are only available via the intravenous route and the liposomal formulations are generally extremely expensive with equivalent or poorer outcomes compared to voriconazole.